The liver is a vital body organ engaged in the detoxification of the body wastes, production of blood clotting & and anti-clotting factors. Sudden rapid disruption of such functions leads to acute liver failure. Artificial Liver Support is provided till recovery of the liver takes place or Liver transplantation is done.
The rationale for such support in acute liver failure includes:
Toxins Removal: Plasma exchange can help remove toxins and metabolic byproducts that accumulate in the blood due to liver failure. By replacing the patient's plasma, the procedure aims to reduce the concentration of harmful substances.
Immunomodulation: Plasma exchange may have immunomodulatory effects by removing antibodies and immune complexes that could contribute to liver damage. This is particularly relevant in cases where an autoimmune component is suspected.
Coagulation Factor Replacement: Liver failure is often associated with impaired synthesis of clotting factors, leading to a risk of bleeding. Plasma exchange can help replace clotting factors and improve hemostasis.
The management of acute liver failure is typically complex and requires a multidisciplinary approach involving hepatologists, intensivists, and other specialists. Patient assessment for KCH Score or MELD Score helps in objectively monitoring progress along with various biochemical markers.
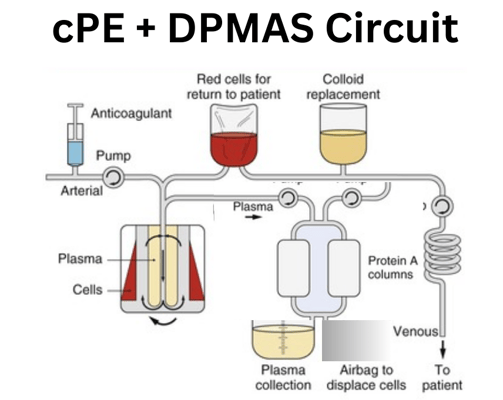
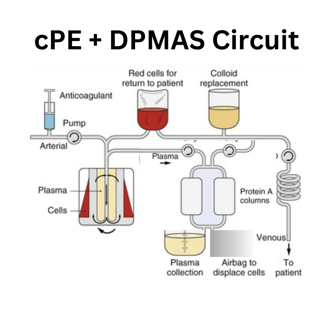
Plasma Exchange, is a medical procedure in which the liquid part of the blood (plasma) is separated from the blood cells, has been considered as the standard line of management for Artificial Liver support in Acute Liver failure. This process involves removing the patient's plasma and replacing it with a replacement fluid, such as albumin or a combination of plasma and a replacement solution. The primary goal of plasma exchange is to remove harmful substances from the blood and replace them with healthier components. However, with the advancing technologies, DPMAS (Double Plasma Membrane Adsorption System) is preferred in ACLF patients. and a 'Hybrid' of Plasma Exchange with DPMAS provides higher maneuverability as per the patient's needs.
The decision to employ plasma exchange is usually made on a case-by-case basis, taking into consideration the underlying cause of liver failure, the patient's clinical condition, and the availability of other treatment options. Apheresis Physicians individualize complex clinical conditions to select modalities and formulate frequency, intensity, and anticoagulation to achieve the decided goals of each procedure as well as contribute to long-term outcomes. The management of acute liver failure is typically complex and requires a multidisciplinary approach involving
Artificial Liver Support Systems
Our mission
We're on a mission to assist the treating physician with optimal patient outcomes with available resources
Our vision
We want to democratize the availability of apheresis technology for patients to live better and healthier lives.
Our team
Our strength lies in our individuality. Set up by Esther Bryce, the team strives to bring in the best talent in various fields, from architecture to interior design and sales.


Esther Bryce
Founder / Interior designer


Lianne Wilson
Broker


Jaden Smith
Architect


Jessica Kim
Photographer
